Do You Have To Use Up All Funds In A Personal Service Contrat To Get Full Medicaid Benifits
one. Medicaid is the nation's public health insurance program for people with low income
Medicaid is the nation's public health insurance plan for people with low income. The Medicaid program covers i in 5 Americans, including many with circuitous and costly needs for care. The programme is the principal source of long-term care coverage for Americans. The vast majority of Medicaid enrollees lack access to other affordable health insurance. Medicaid covers a broad array of health services and limits enrollee out-of-pocket costs. Medicaid finances nearly a 5th of all personal wellness care spending in the U.S., providing pregnant financing for hospitals, customs health centers, physicians, nursing homes, and jobs in the health care sector. Title 19 of the Social Security Act and a large torso of federal regulations govern the program, defining federal Medicaid requirements and state options and authorities. The Centers for Medicare and Medicaid Services (CMS) within the Department of Wellness and Human being Services (HHS) is responsible for implementing Medicaid (Effigy i).
Figure one: Medicaid plays a central role in our health intendance system.
2. Medicaid is structured as a federal-state partnership
Subject to federal standards, states administrate Medicaid programs and take flexibility to determine covered populations, covered services, wellness care commitment models, and methods for paying physicians and hospitals. States can besides obtain Section 1115 waivers to test and implement approaches that differ from what is required by federal statute but that the Secretary of HHS determines advance plan objectives. Because of this flexibility, there is significant variation across country Medicaid programs.
The Medicaid entitlement is based on two guarantees: first, all Americans who run into Medicaid eligibility requirements are guaranteed coverage, and second, states are guaranteed federal matching dollars without a cap for qualified services provided to eligible enrollees. The match rate for well-nigh Medicaid enrollees is determined past a formula in the law that provides a match of at least 50% and provides a higher federal friction match rate for poorer states (Figure two).

Figure 2: The basic foundations of Medicaid are related to the entitlement and the federal-state partnership.
3. Medicaid coverage has evolved over fourth dimension
Under the original 1965 Medicaid law, Medicaid eligibility was tied to cash assistance (either Aid to Families with Dependent Children (AFDC) or federal Supplemental Security Income (SSI) starting in 1972) for parents, children and the poor aged, blind and people with disabilites. States could opt to provide coverage at income levels to a higher place greenbacks help. Over time, Congress expanded federal minimum requirements and provided new coverage options for states especially for children, pregnant women, and people with disabilities. Congress also required Medicaid to aid pay for premiums and price-sharing for low-income Medicare beneficiaries and allowed states to offering an option to "buy-in" to Medicaid for working individuals with disabilities. Other coverage milestones included severing the link between Medicaid eligibility and welfare in 1996 and enacting the Children's Health Insurance Program (Bit) in 1997 to comprehend low-income children above the cut-off for Medicaid with an enhanced federal match rate. Following these policy changes, for the first time states conducted outreach campaigns and simplified enrollment procedures to enroll eligible children in both Medicaid and CHIP. Expansions in Medicaid coverage of children marked the starting time of after reforms that recast Medicaid equally an income-based health coverage programme.
In 2010, as part of a broader wellness coverage initiative, the Affordable Intendance Act (ACA) expanded Medicaid to nonelderly adults with income up to 138% FPL ($17,236 for an individual in 2019) with enhanced federal matching funds (Figure 3). Prior to the ACA, individuals had to be categorically eligible and meet income standards to qualify for Medicaid leaving well-nigh low-income adults without coverage options equally income eligibility for parents was well beneath the federal poverty level in most states and federal law excluded adults without dependent children from the program no matter how poor. The ACA changes finer eliminated categorical eligibility and allowed adults without dependent children to be covered; however, as a result of a 2012 Supreme Court ruling, the ACA Medicaid expansion is effectively optional for states. Under the ACA, all states were required to modernize and streamline Medicaid eligibility and enrollment processes. Expansions of Medicaid have resulted in celebrated reductions in the share of children without coverage and, in the states adopting the ACA Medicaid expansion, sharp declines in the share of adults without coverage. Many Medicaid adults are working, simply few accept access to employer coverage and prior to the ACA had no options for affordable coverage.

Figure 3: Medicaid has evolved over time to meet changing needs.
4. Medicaid covers 1 in 5 Americans and serves diverse populations
Medicaid provides health and long-term care for millions of America's poorest and near vulnerable people, interim as a loftier risk pool for the private insurance marketplace. In FY 2017, Medicaid covered over 75 one thousand thousand low-income Americans. As of February 2019, 37 states have adopted the Medicaid expansion. Data as of FY 2017 (when fewer states had adopted the expansion) show that 12.6 one thousand thousand were newly eligible in the expansion group. Children account for more than iv in x (43%) of all Medicaid enrollees, and the elderly and people with disabilities account for about one in 4 enrollees.
Medicaid plays an particularly critical office for sure populations roofing: near half of all births in the typical state; 83% of poor children; 48% of children with special wellness care needs and 45% of nonelderly adults with disabilities (such every bit physical disabilities, developmental disabilities such as autism, traumatic encephalon injury, serious mental illness, and Alzheimer's affliction); and more vi in ten nursing habitation residents. States can opt to provide Medicaid for children with significant disabilities in college-income families to fill gaps in private health insurance and limit out-of-pocket financial burden. Medicaid also assists nearly 1 in v Medicare beneficiaries with their Medicare premiums and cost-sharing and provides many of them with benefits not covered by Medicare, especially long-term care (Figure four).
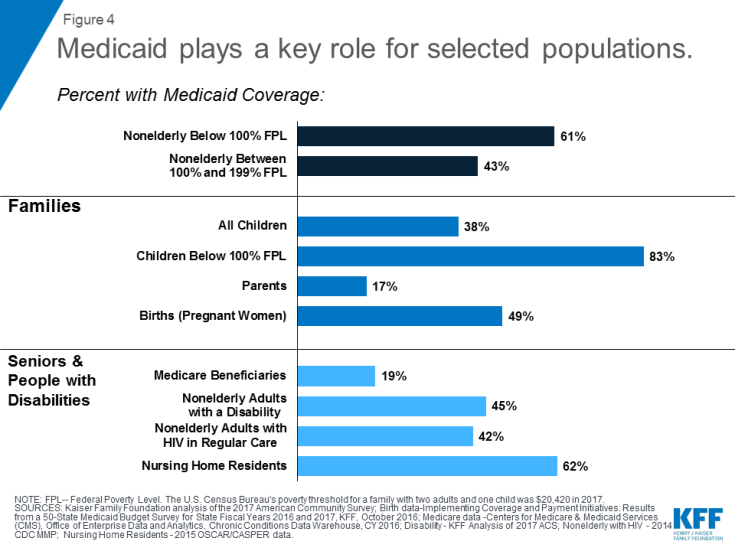
Figure 4: Medicaid plays a key role for selected populations.
5. Medicaid covers a broad range of health and long-term care services
Medicaid covers a broad range of services to address the various needs of the populations it serves (Figure 5). In addition to covering the services required by federal Medicaid police force, many states elect to cover optional services such equally prescription drugs, concrete therapy, eyeglasses, and dental care. Coverage for Medicaid expansion adults contains the ACA's ten "essential health benefits" which include preventive services and expanded mental health and substance use treatment services. Medicaid plays an important role in addressing the opioid epidemic and more broadly in connecting Medicaid beneficiaries to behavioral wellness services. Medicaid provides comprehensive benefits for children, known as Early Periodic Screening Diagnosis and Treatment (EPSDT) services. EPSDT is especially of import for children with disabilities because private insurance is often inadequate to meet their needs. Dissimilar commercial health insurance and Medicare, Medicaid also covers long-term care including both nursing home care and many habitation and customs-based long-term services and supports. More than one-half of all Medicaid spending for long-term care is at present for services provided in the home or community that enable seniors and people with disabilities to live independently rather than in institutions.
Given that Medicaid and Chip enrollees have express power to pay out-of-pocket costs due to their modest incomes, federal rules prohibit states from charging premiums in Medicaid for beneficiaries with income less than 150% FPL, prohibit or limit toll sharing for some populations and services, and limit full out-of-pocket costs to no more than 5% of family income. Some states take obtained waivers to accuse higher premiums and toll sharing than immune under federal rules. Many of these waivers target expansion adults but some also use to other groups eligible through traditional eligibility pathways.

Figure five: Medicaid'south benefits reflect the needs of the population it serves.
six. Near Medicaid enrollees get care through private managed care plans
Over 2-thirds of Medicaid beneficiaries are enrolled in private managed care plans that contract with states to provide comprehensive services, and others receive their intendance in the fee-for-service arrangement (Figure 6). Managed care plans are responsible for ensuring admission to Medicaid services through their networks of providers and are at fiscal adventure for their costs. In the past, states express managed care to children and families, but they are increasingly expanding managed care to individuals with complex needs. Close to half united states of america now cover long-term services and supports through risk-based managed intendance arrangements. Most states are engaged in a diversity of delivery system and payment reforms to control costs and improve quality including implementation of patient-centered medical homes, better integration of physical and behavioral wellness intendance, and development of "value-based purchasing" approaches that tie Medicaid provider payments to health outcomes and other performance metrics. Community health centers are a central source of chief intendance, and safety-net hospitals, including public hospitals and academic medical centers, provide a lot of emergency and inpatient hospital care for Medicaid enrollees.
Medicaid covers a continuum of long-term services and supports ranging from home and community-based services (HCBS) that allow persons to live independently in their ain homes or in other community settings to institutional care provided in nursing facilities (NFs) and intermediate intendance facilities for individuals with intellectual disabilities (ICF-IDs). In FY 2016, HCBS represented 57 percent of total Medicaid expenditures on LTSS while institutional LTSS represented 43 pct. This is a dramatic shift from 1995 (two decades earlier) when institutional settings deemed for 82 percent of national Medicaid LTSS expenditures.

Effigy vi: Over two-thirds of all Medicaid beneficiaries receive their care in comprehensive risk-based MCOs.
7. Medicaid facilitates admission to care
A big torso of research shows that Medicaid beneficiaries accept far better admission to care than the uninsured and are less probable to postpone or go without needed intendance due to toll. Moreover, rates of access to care and satisfaction with care amid Medicaid enrollees are comparable to rates for people with private insurance (Effigy 7). Medicaid coverage of low-income pregnant women and children has contributed to dramatic declines in babe and kid mortality in the U.Southward. A growing trunk of enquiry indicates that Medicaid eligibility during childhood is associated with reduced teen mortality, improved long-run educational attainment, reduced disability, and lower rates of hospitalization and emergency department visits in later life. Benefits also include 2d-gild fiscal effects such as increased taxation collections due to higher earnings in adulthood. Research findings prove that state Medicaid expansions to adults are associated with increased access to intendance, improved cocky-reported health, and reduced mortality amongst adults.
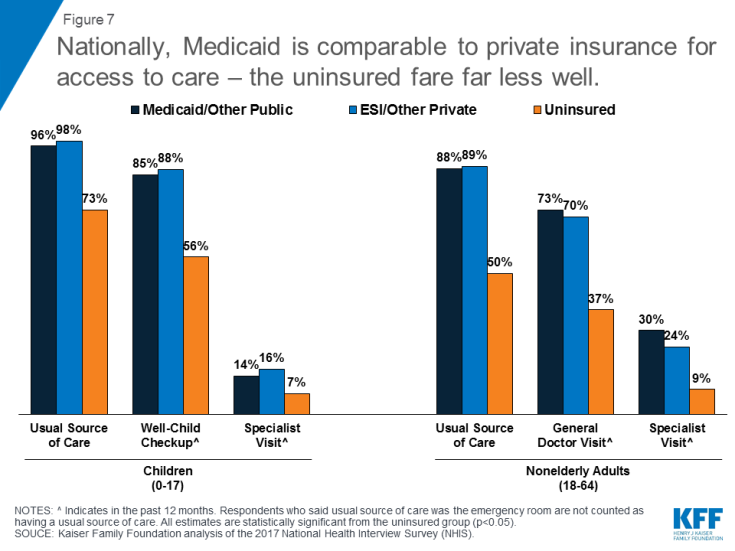
Figure 7: Nationally, Medicaid is comparable to private insurance for access to intendance – the uninsured fare far less well.
Gaps in access to certain providers, especially psychiatrists, some specialists, and dentists, are ongoing challenges in Medicaid and often in the wellness system more broadly due to overall provider shortages, and geographic maldistribution of health intendance providers. Nevertheless, depression Medicaid payment rates have long been associated with lower doc participation in Medicaid, especially amidst specialists. Managed intendance plans, which now serve almost Medicaid beneficiaries, are responsible under their contracts with states for ensuring adequate provider networks. There is no evidence that physician participation in Medicaid is failing. In a 2015 survey, 4 in 10 principal care providers who accepted Medicaid reported seeing an increased number of Medicaid patients since January 2014, when the coverage expansions in the ACA took total outcome.
Medicaid covers people who are struggling with opioid addiction and enhances state capacity to provide access to early interventions and treatment services. The Medicaid expansion, with enhanced federal funding, has provided states with additional resources to cover many adults with addictions who were previously excluded from the program. Medicaid covers 4 in 10 nonelderly adults with opioid addiction.
8. Medicaid is jointly financed by states and the federal government
Medicaid is financed jointly by the federal government and states. The federal government matches land Medicaid spending. The federal match rate varies by land based on a federal formula and ranges from a minimum of 50% to nearly 75% in the poorest country. Under the ACA, the federal lucifer rate for adults newly eligible was 100% for 2014-2016, phasing downwardly gradually to xc% in 2020 and thereafter (93% in 2019). The federal matching structure provides states with resource for coverage of their low-income residents and also permits country Medicaid programs to reply to demographic and economic shifts, changing coverage needs, technological innovations, public health emergencies such as the opioid addiction crunch, and disasters and other events beyond states' control. The guaranteed availability of federal Medicaid matching funds eases budgetary pressures on states during recessionary periods when enrollment rises. Federal matching rates practise non automatically adjust to economic shifts but Congress has twice raised them temporarily during downturns to strengthen support for states.
Full federal and state Medicaid spending was $577 billion in FY 2017. Medicaid is the 3rd-largest domestic plan in the federal upkeep, later Social Security and Medicare, bookkeeping for 9.five% of federal spending in FY 2017. In 2017, Medicaid was the second-largest item in land budgets, after uncomplicated and secondary didactics (Effigy 8).
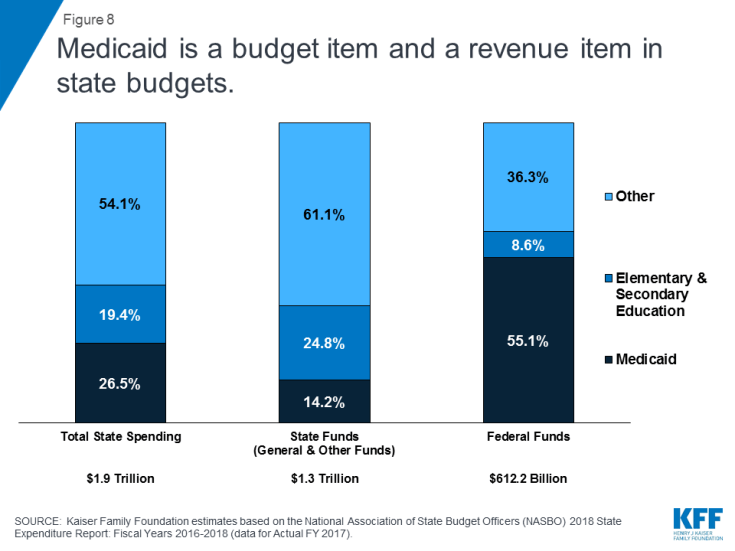
Figure viii: Medicaid is a budget item and a revenue item in country budgets.
Federal Medicaid matching funds are the largest source of federal revenue (55.1%) in state budgets. Accounting for state and federal funds, Medicaid accounts for 26.v% of total country spending. Because Medicaid plays a big role in state budgets, states take an interest in price containment and program integrity. Enrollment and spending increased significantly following implementation of the ACA, but accept moderated in more than recent years. While slower caseload growth helped to mitigate Medicaid spending growth in FYs 2018 and 2019, higher costs for prescription drugs, long-term services and supports and behavioral wellness services, and policy decisions to implement targeted provider rate increases were cited every bit factors putting up pressures on Medicaid spending.
ix. Medicaid spending is concentrated on the elderly and people with disabilities
Seniors and people with disabilities brand up 1 in 4 beneficiaries but business relationship for almost two-thirds of Medicaid spending, reflecting loftier per enrollee costs for both acute and long-term care (Effigy 9). Medicaid is the primary payer for institutional and community-based long-term services and support – as at that place is limited coverage under Medicare and few affordable options in the private insurance market. Over half of Medicaid spending is attributable to the highest-cost 5 percentage of enrollees. Nonetheless, on a per-enrollee basis, Medicaid is low-toll compared to private insurance, largely due to lower Medicaid payment rates for providers. Analysis shows that if adult Medicaid enrollees had job-based coverage instead, their average health care costs would be more than 25% higher. Medicaid spending per enrollee has also been growing more slowly than private insurance premiums and other health spending benchmarks.
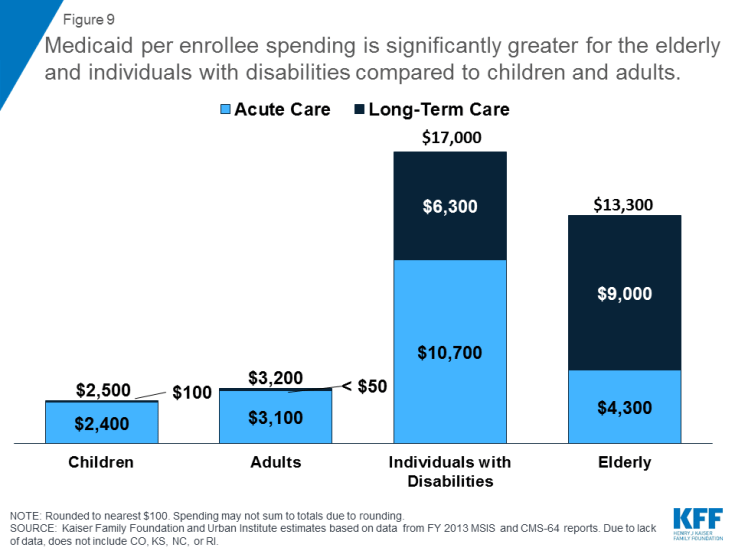
Figure ix: Medicaid per enrollee spending is significantly greater for the elderly and individuals with disabilities compared to children and adults.
10. The bulk of the public holds favorable views of Medicaid
Public opinion polling suggests that Medicaid has broad support. 7 in x Americans say they accept ever had a connection with Medicaid including iii in ten who were e'er covered themselves. Fifty-fifty across political parties, majorities have a favorable opinion of Medicaid and say that the program is working well (Figure 10). In addition, polling shows that few Americans want decreases in federal Medicaid funding. In addition to broad-based support, Medicaid has very strong support among those who are disproportionately served by Medicaid including children with special health care needs, seniors, and people with disabilities.
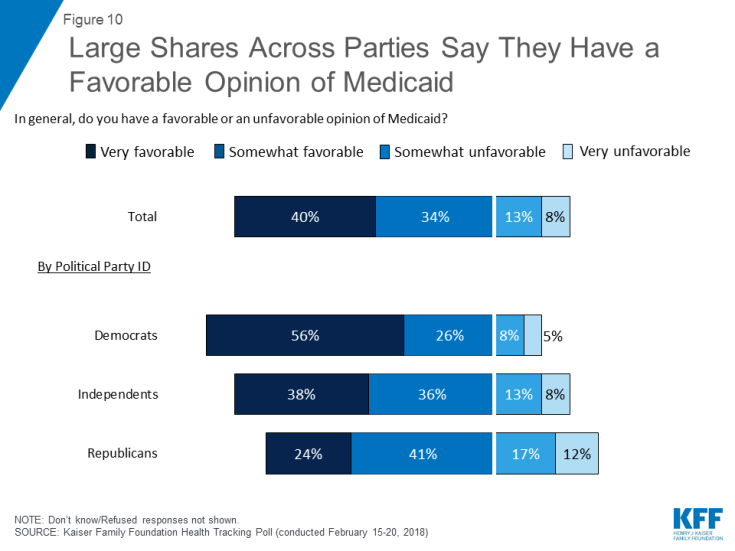
Figure 10: Large Shares Across Parties Say They Have a Favorable Opinion of Medicaid
Conclusion
Medicaid provides comprehensive coverage and financial protection for millions of Americans, near of whom are in working families. Despite their low income, Medicaid enrollees experience rates of access to care comparable to those amid people with private coverage. In addition to astute health care, Medicaid covers plush long-term care for millions of seniors and people of all ages with disabilities, in both nursing homes and the community. Medicaid bolsters the private insurance market by interim as a loftier-take chances pool providing coverage for many uninsured people who were excluded from the private, largely employment-based health insurance system because of low income, poor health status, or disability. Medicaid also supports Medicare by helping low-income Medicare beneficiaries pay for premiums and price-sharing and providing long-term services and supports that are not covered past Medicare.
Accounting for one-5th of health care spending, Medicaid funding is a major source of support for hospitals and physicians, nursing homes, and jobs in the health intendance sector. The guarantee of federal matching funds on an open-ended basis allows states the flexibility to utilize Medicaid to address wellness priorities such as addressing the opioid epidemic. The financing construction also provides support for states to allow Medicaid to operate equally safe net when economic shifts and other dynamics crusade coverage needs to grow.
Every bit Medicaid plays a large function in both federal and land budgets and is the chief source of coverage for depression-income Americans, it is a constant source of contend. Efforts to repeal and supersede the ACA besides included primal reforms to Medicaid to cap federal financing through a block grant or per capita cap. Such proposals were narrowly defeated in 2017. Important Medicaid issues to watch in 2019 include Medicaid expansion developments and continued focus on changing the program through Medicaid demonstration waiver activities, including those focused on work requirements and other eligibility restrictions besides every bit potential waivers to reshape Medicaid financing. In addition, other areas in Medicaid to watch are reforms in benefits, payment and delivery systems, efforts to address social determinants of health, efforts to control prescription drug costs, and expand capacity to accost the opioid epidemic and provide community based long-term care services. Congress and states could likewise consider broader health reform that could expand the function of public programs in wellness care including Medicare for All or Medicaid buy-in programs that could have significant implications for Medicaid.
Do You Have To Use Up All Funds In A Personal Service Contrat To Get Full Medicaid Benifits,
Source: https://www.kff.org/medicaid/issue-brief/10-things-to-know-about-medicaid-setting-the-facts-straight/
Posted by: stroudsoublartand.blogspot.com


0 Response to "Do You Have To Use Up All Funds In A Personal Service Contrat To Get Full Medicaid Benifits"
Post a Comment